Abstract
A low intake of calcium is widely considered to be a risk factor for future fracture. The aim of this study was to quantify this risk on an international basis and to explore the effect of age, gender and bone mineral density (BMD) on this risk. We studied 39,563 men and women (69% female) from six prospectively studied cohorts comprising EVOS/EPOS, CaMos, DOES, the Rotterdam study, the Sheffield study and a cohort from Gothenburg. Cohorts were followed for 152,000 person-years. The effect of calcium intake as judged by the intake of milk on the risk of any fracture, any osteoporotic fracture and hip fracture alone was examined using a Poisson model for each sex from each cohort. Covariates examined were age and BMD. The results of the different studies were merged by using the weighted β-coefficients. A low intake of calcium (less than 1 glass of milk daily) was not associated with a significantly increased risk of any fracture, osteoporotic fracture or hip fracture. There was no difference in risk ratio between men and women. When both sexes were combined there was a small but non-significant increase in the risk of osteoporotic and of hip fracture. There was also a small increase in the risk of an osteoporotic fracture with age which was significant at the age of 80 years (RR=1.15; 95% CI=1.02–1.30) and above. The association was no longer significant after adjustment for BMD. No significant relationship was observed by age for low milk intake and hip fracture risk. We conclude that a self-reported low intake of milk is not associated with any marked increase in fracture risk and that the use of this risk indicator is of little or no value in case-finding strategies.
Similar content being viewed by others
Introduction
Calcium nutrition is commonly considered to be important for the attainment of peak bone mass [1,2,3,4,5]. In later life many, but not all, observational studies have shown an association between intake of calcium and fracture risk but the causality of any such association is also controversial [6,7]. Nevertheless, a low calcium intake is regarded as a risk factor for fracture, in part due to the fact that the recommended nutrient intake (RNI) for calcium is widely considered to be between 750 and 1000 mg daily [8,9] and even higher (1200–1500 mg daily) in the US [10,11], whereas the dietary intake is substantially less in most regions of the world.
The causality of any association is strengthened by observations that the administration of calcium with vitamin D has been shown to decrease fracture risk, particularly in the elderly and those with the lower intakes of calcium [12,13,14]. These trials included vitamin D, however, and the separate effects of calcium and vitamin D alone are less secure. In a recent meta-analysis of 15 prospective studies of at least 1 year duration, calcium supplements significantly decreased the rate of bone loss at all skeletal sites. Fractures were few and, although the combined point estimate of relative risk was below unity in the five studies with this outcome (0.77 for vertebral fractures and 0.86 for non-vertebral fractures), and the effect was not significant [15].
At present, assessment guidelines do not include a low dietary intake of calcium as a risk factor for case finding strategies [9,16,17,18,19,20]. The question arises whether a low intake of calcium can be utilised as a risk factor to characterise probability of fracture. The aim of the present study was to quantify the fracture risk associated with a low dietary intake of calcium as judged by self-reported intake of milk in an international setting and to explore the dependence of this risk with age, sex and BMD.
Materials and methods
We studied 39,563 men and women taken from six prospectively studied cohorts drawn randomly from populations in Europe, Australia and Canada as part of a collaborative study to identify clinical risk factors for fracture. These comprise the EVOS/EPOS study, CaMos, DOES, the Rotterdam Study, the Sheffield Study and a cohort from Gothenburg. Brief details of the cohorts studied are given below and summarised in Table 1.
EVOS/EPOS
The European Vertebral Osteoporosis Study (EVOS) comprised age- and sex-stratified random samples from 36 centres in 19 European countries [21]. Equal numbers of men and women were drawn in each centre within six 5-year age bands (50–74 up to 75–79 years). A base-line radiograph for vertebral fracture prevalence was undertaken in 15,570 men and women with a response rate of 29%. Bone mineral density was measured in 4574 men and women from 13 centers by DXA at the femoral neck using pencil beam machines that were cross-calibrated using the European spine phantom. The sample provided the framework for the European Prospective Osteoporosis study (EPOS) where repeated assessment was undertaken in 29 of the centers [22,23]. For this analysis validated follow-up was available for 13,445 men and women with an average follow-up time of 3 years. Bone mineral density measurements were undertaken in 4574 men and women.
CaMos
The Canadian Multicentre Osteoporosis Study (CaMos) is an on-going prospective age-stratified and population-based cohort. The study is documenting the incidence of fractures and risk factors in a random sample of 9401 men and women aged 25 years or more selected by telephone listings. The sampling frame is from nine study centers in seven provinces with a response rate of 47% [24]. Characterisation of individuals was by interview. Bone mineral density was measured by DXA at the hip in 8317 men and women at seven centers with the Hologic QDR 1000, and the Lunar-DPX Alpha at two centers. Machines were cross-calibrated using the European spine phantom. For this analysis, validated fracture follow up was available for 9401 participants (2914 men) with an average follow up time of 3 years.
DOES
The Dubbo Osteoporosis Epidemiology Study (DOES) is a population based study with multiple assessments of skeletal status in men and women aged 60 years or more from Dubbo, Australia [25]. Participation in the study was 56% of the population. Baseline measurements included BMD at the femoral neck assessed using DXA (GE-Lunar DPX). Fractures were identified through radiologists’ reports from the two centers servicing the region. Validated fracture follow-up was available for 2065 participants (805 men) with an average follow up of 8 years. Femoral neck BMD was measured at baseline in 2065 individuals (808 men).
The Rotterdam Study
The Rotterdam study, begun in 1990, is an ongoing prospective cohort study that aimed to examine and follow-up all residents aged 55 years and older living in Ommoord, a district of Rotterdam [26]. By 1993, 7983 residents had been included (response rate 78%). Bone mineral density was assessed at the femoral neck by DXA using a Lunar DPX-L. Fracture follow-up was undertaken using an automated link with general practitioner computer systems and hospital admission data [27]. Fracture data were collected and validated by two independent research physicians. For this analysis, validated fracture follow up was available for 5408 participants (2220 men) with an average follow up time of 6 years. Femoral neck BMD was measured in 4979 individuals (2060 men).
The Sheffield Study
The Sheffield cohort comprised women aged 75 years or more selected randomly from the population of Sheffield, UK, and surrounding districts between 1993 and 1999. Approximately 35,000 women, identified from general practitioner listings, were contacted by letter and invited to attend for assessment of their skeletal status. A total of 5873 women were willing to attend for the screening visit. Of these, 281 were excluded, and the remainder randomly allocated after informed consent to treatment with the bisphosphonate clodronate, or to an identical placebo. The material used for the present paper comprised 2173 women allocated to treatment with placebo [28]. All but 22 women had a baseline assessment of bone mineral density undertaken at the femoral neck using the Hologic 4500. Outcomes were assessed by 6-monthly home visits.
Gothenburg II
The Gothenburg study comprised a randomly drawn population cohort of women aged 21–89 years with a mean follow-up of up to 8 years (mean 3.8 years) [29]. Seventy percent of those invited participated in the baseline investigation, which comprised a standardised questionnaire for risk factors and a BMD at the distal forearm using the OsteoMeter DTX 200. Validated fracture follow-up was available in 7071 women and BMD measurements in 7062.
Baseline and outcome variables
The construct of the question to determine intake of milk differed between the cohorts studied. Where glasses of milk were recorded (EVOS/EPOS, CaMos, Sheffield, Gothenburg) an intake of less than 1 glass of milk a day was taken as the level to dichotomise the intake of milk (approximately 250 mg calcium daily or less). The size of glass was not standardised. The choice of cut-off was pragmatic but corresponds to the intake below which a large case control study indicated a significant increase in hip fracture risk [30]. In the case of Rotterdam and DOES, total calcium intake was recorded by a food frequency questionnaire. A threshold of <500 mg of calcium was used in these cohorts to dichotomise the variable on the assumption that approximately 50% of calcium intake is in the form of milk in these countries [31,32]. Where intake was recorded at different ages of life we utilised current intake of milk.
Prospective fracture ascertainment was undertaken by self-report (Sheffield, EVOS/EPOS), and/or verified from hospital central data-bases (EVOS/EPOS, CaMos, DOES, Rotterdam, Sheffield and Gothenburg II). Fractures considered to be due to osteoporosis were analysed and in addition hip fracture alone was considered separately. An osteoporotic fracture was one considered to be due to osteoporosis by the investigator. For the EVOS study osteoporotic fractures comprised hip, forearm, humeral or clinical spine fractures. For the CaMos study, they comprised fractures of the spine, pelvis, ribs, distal forearm, forearm and hip. In the other cohorts (Sheffield, Rotterdam, Gothenburg, DOES) fractures at sites considered to be characteristic for osteoporosis were extracted which, in addition to the sites above, included fractures of the proximal humerus, other femoral fractures, clavicle, scapula and tibial fractures in women [33].
Statistical methods
The risk of fracture was estimated by Poisson regression applied to each cohort and each sex separately. Covariates included current time, current age, milk intake and milk intake times current age. Since risk assessment with clinical risk factors may be undertaken with or without the use of BMD [28], an additional model included the covariates above with bone mineral density. Bone mineral density was undertaken at the femoral neck by DXA with the exception of the Gothenburg cohort which measured bone mineral density at the distal forearm using the DTX-200 Osteometer.
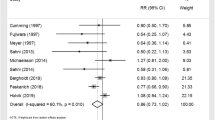
The beta coefficients of each cohort for each sex were weighted according to the variance and merged to determine the weighted mean and standard deviation. The risk ratio of those on low calcium intakes versus those on higher calcium intakes was equal to emean. Heterogeneity was tested by the I2 statistic [34]. There was no significant heterogeneity between cohorts (P>0.3; I2=13; 95% confidence interval=0–54% for osteoporotic fracture and I2=0, 0–25% for hip fracture), and a fixed effects model was used.
Results
The total sample studied was 39,563 men and women followed for 151,957 person years (Table 1). During this time there were 3191 fractures, 2469 fractures thought to be related to osteoporosis, including 413 hip fractures. Bone mineral density measurements were available in 74% of individuals.
A low intake of milk was not associated with a significantly increased risk of osteoporotic fracture or of hip fracture. There was no difference in risk ratio between men and women (Table 2).
When risk ratio was examined by age in men and women combined, a low intake of milk was associated with an increased risk of osteoporotic fracture only from the age of 80 years. With all ages combined the risk ratio (1.10) was of borderline significance (95% CI=1.00–1.21; P=0.056). The association was no longer significant when adjusted for BMD (Table 3). For hip fracture, low intake of milk was not associated with an increased risk at any age, both with and without adjustment for BMD (Table 4). For any fracture, there was no association of low milk intake with fracture risk (data not shown).
The exclusion of the Gothenburg cohort, in which BMD was assessed at the forearm, made no difference to the overall conclusions (data not shown).
There was a weak but highly significant correlation between intake of milk and BMD (r=0.0364; P=4.5×10−10).
Discussion
The principal finding of the present study undertaken in large and internationally drawn cohorts is that a low intake of calcium, as judged by the intake of milk, does not confer a substantial increase in fracture risk. No significant association was noted between intake of milk and the risk of hip fracture at any age and in either sex. For osteoporotic fractures (but not for hip fracture alone), a small, but significant risk was found from the age of 80 years, but not in younger individuals. The association was no longer significant when adjusted for BMD. These results are in agreement with results reported from a large prospective cohort of more than 60,000 women aged 40–74 years from central Sweden in whom more than 1500 hip fractures and 4000 osteoporotic fractures were studied. The age adjusted relative risk of hip fracture was 1.01 (95% CI=0.96–1.06) per 300 mg calcium/day and for all osteoporotic fractures 0.99 (0.96–1.03) [35]. They also accord with meta-analyses of other prospective studies of dietary intake [36] or calcium supplementation [15], although a non-significant trend for a reduction in vertebral and non-vertebral fracture was observed. It is of interest that intake of milk correlated significantly with BMD. The correlation was, however, low with a coefficient of determination of 0.13%. From the correlation coefficient, it can be calculated that a sample size of >500,000 would be required to show a relationship between milk intake and fracture risk. This is probably an underestimate, since the correlation was computed from the dichotomous variable that overestimates the true correlation coefficient.
The strength of the present study is that the estimate of risk is derived from several prospective studies of randomly selected population cohorts from a wide geographical distribution. The same cohorts have been used to assess the effects of prior corticosteroid use, low body mass index and prior fracture on fracture risk and these have shown significant associations that lend credibility to the suitability of these cohorts for the identification of risk factors for fracture [37,38,39]. One limitation of the study is the construct of the question concerning calcium intake, which differed somewhat between cohorts and at best lacks precision and accuracy. Although total calcium intake was recorded in two of the studies and would have included calcium supplements, in other cohorts calcium supplements may have confounded the relationship between intake of milk and total intake of calcium. The effect of this heterogeneity is likely to weaken any association. Moreover, we were unable, using the construct of the question, to examine intakes of calcium lower than 500 mg daily, so that we cannot exclude a threshold effect as has been shown in case control studies for hip fracture risk [30,40], albeit with a threshold similar to the one that we used to dichotomise milk intake. Finally, we neglected sources of calcium intake other than milk, including cheese and yoghurt, and variations in dietary vitamin D or sunlight exposure [30,40,41]. This study should not, therefore, be misinterpreted as suggesting no causative role of calcium in the causation of fractures, nor a role for calcium nutrition in their prevention. Indeed, the association of an increased risk of osteoporotic fracture in the elderly is consistent with an important role for calcium in the elderly in whom other risk factors are more prevalent including immobility and lack of sunlight exposure.
Notwithstanding, the aim of the study was to determine the suitability of the use of calcium intake, as judged by intake of milk, as a risk factor for patient assessment by general physicians alongside the elucidation of other clinical risk factors. In this context, the use of more accurate but more complex instruments to determine intake is likely to be unfeasible in a general practice setting.
We conclude that if habitual dietary intake of calcium is a significant risk factor for fractures, a simple questionnaire on the intake of milk is unlikely to be of value as an adjunct to case finding.
References
Heaney RP (1993) Nutritional factors in osteoporosis. Ann Rev Nutr 13:287–316
Valimaki MJ, Karkkainen M, Lamberg-Allardt C, Laitinen K, Heikkinen J (1994) Exercise, smoking and calcium intake during adolescence and early adulthood as determinants of peak bone mass. BMJ 309:230–235
Bonjour JP, Carrie AL, Ferrari S et al. (1997) Calcium enriched foods and bone mass growth in prepubertal girls: a randomised, double-blind, placebo-controlled trial. J Clin Invest 99:1287–1294
Kanis JA, Passmore R (1989) Calcium supplementation of the diet not justified by the present evidence. BMJ 298:137–140 and 205–208
Nordin BEC, Heaney RP (1990) Calcium supplementation of the diet: justified by the present evidence. BMJ 300:1056–1060
Cumming R, Cummings S, Nevitt M, Scott J, Ensrud K, Vogt T, Fox K (1997) Calcium intake and fracture risk: results from the study of osteoporotic fractures. Am J Epidemiol 145:927–935
Kanis JA (1999) The use of calcium in the management of osteoporosis. Bone 24:279–290
Yates AA, Schlicker SA, Suitor CW (1998) Dietary reference intakes: the new basis for recommendations for calcium and related nutrients, B vitamins, and choline. J Am Diet Assoc 98:699–706
European Commission (1998) Report on osteoporosis in the European Community—action on prevention. Luxembourg Office for Official Publications of the European Communities, pp 112
National Osteoporosis Foundation (1998) Physician’s guide to prevention and treatment of osteoporosis. National Osteoporosis Association, Washington D.C., pp 1–38
National Institutes of Health (2001) Osteoporosis prevention, diagnosis and therapy. NIH consensus development conference statement. JAMA 285:785–795
Chapuy MC, Arlot ME, Delmas PD, Meunier PJ (1994) Effect of calcium and cholecalciferol treatment for three years on hip fractures in elderly women. BMJ 308:1081–1082
Chapuy MC, Arlot ME, Duboeuf F, Brun J, Crouzet B, Arnaud S, Delmas PD, Meunier PJ (1992) Vitamin D3 and calcium to prevent hip fractures in elderly women. N Engl J Med 327:1637–1642
Dawson-Hughes B, Harris SS, Krall EA, Dallal GE (1997) Effect of calcium and vitamin D supplementation on bone density in men and women 65 years of age or older. N Engl J Med 337:670–676
Shea B, Wells G, Cranney A, Zytaruk N, Robinson V, Griffith L, Ortiz Z, Peterson J, Adachi J, Tugwell P, Guyatt G, the Osteoporosis Methodology Group and the Osteoporosis Research Advisory Group (2002) Meta-analysis of calcium supplementation for the prevention of postmenopausal osteoporosis. Endocr Rev 23:552–559
American College of Rheumatology, Ad Hoc Committee on glucocorticosteroid-induced osteoporosis (2001) Recommendations for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthr Rheum 44:1496–1503
Bone and Tooth Society of Great Britain, National Osteoporosis Society and Royal College of Physicians (2002) Guidelines on the prevention and treatment of glucocorticoid-induced osteoporosis. Royal College of Physicians, London
Kanis JA, Delmas P, Burckhardt P, Cooper C, Torgerson D on behalf of the EFFO (1997) Guidelines for the diagnosis and management of osteoporosis. Osteoporos Int 7:390–406
Royal College of Physicians (1999) Osteoporosis: clinical guidelines for prevention and treatment. Royal College of Physicians, London
Royal College of Physicians (2000) Osteoporosis: clinical guidelines for prevention and treatment. Update on pharmacological interventions and an algorithm for management. Royal College of Physicians, London
O’Neill TW, Felsenberg D, Varlow J, Cooper C, Kanis JA, Silman AJ (1996) The prevalence of vertebral deformity in European men and women: the European Vertebral Osteoporosis Study. J Bone Miner Res 11:1010–1017
Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ, Reeve J, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Delmas PD, Dequeker J, Dilsen G, Falch JA, Felsch B, Felsenberg D, Finn JD, Gennari C, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopez Vaz A, Lorenc R, Lyritis G, Marchand F, Masaryk P, Matthis C, Miazgowski T, Naves-Diaz M, Pols HAP, Poor G, Rapado A, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, O’Neill TW (2002) Incidence of limb fracture across Europe: results from the European prospective osteoporosis study EPOS. Osteoporos Int 13:565–571
Felsenberg D, Silman AJ, Lunt M, Ambrecht G, Ismail AA, Finn JD, Cockerill WC, Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper C, Dequeker J, Eastell R, Ershova O, Felsch B, Gowin W, Havelka S, Hoszowski K, Jajic I, Janot J, Johnell O, Kanis JA, Kragl G, Lopez Vaz A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi G, Pols HAP, Poor G, Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, Weber K, Woolf AD, Reeve J, O’Neill TW (2002) Incidence of vertebral fracture in Europe: results from the European Prospective Osteoporosis Study EPOS. J Bone Miner Res 17:716–724
Kreiger N, Tenenhouse A, Joseph L et al. (1999) The Canadian Multicentre Osteoporosis Study CaMos: background, rationale, methods. Can J Ageing 18:376–387
Jones G, Nguyen TV, Sambrook PN, Kelly PJ, Gilbert C, Eisman JA (1994) Symptomatic fracture incidence in elderly men and women. The Dubbo osteoporosis Epidemiology Study DOES. Osteoporos Int 4:277–282
Hofman A, Grobbee DE, de Jong PT, van den Ouweland FA (1991) Determinants of disease and disability in the elderly: The Rotterdam Elderly Study. Eur J Epidemiol 7:403–422
De Laet CEDH, Van Hout BA, Burger H, Hofman A, Weel AEAM, Pols HAP (1998) Hip fracture prediction in elderly men and women: validation of the Rotterdam Study. J Bone Miner Res 13:1587–1593
Johansson H, Oden A, Johnell O, Jonsson B, De Laet C, Oglesby A, McCloskey EV, Kayan K, Jalava T, Kanis JA (2004) Optimisation of BMD measurements to identify high risk groups for treatment—a test analysis. J Bone Miner Res (in press)
Senstrom M, Olsson J-O, Mellstrom D (2000) Thyroid hormone replacement is not related to increased risk of osteoporosis. Osteoporos Int 11:S144
Johnell O, Gullberg B, Kanis JA, Allander E, Elffors L, Dequeker J, Dilsen G, Gennari C, Lopez Vaz A, Lyritis G, Mazzuoli G, Miravet L, Passeri M, Perez-Cano R, Rapido A, Ribot C (1995) Risk factors for hip fracture in European women. The MEDOS study. J Bone Miner Res 10:1802–1815
Krough V, Frendenheim JL, D’Amacis A, Scaccini C, Sette S, Ferro-Luzzi A, Trevisan M (1993) Food sources of nutrients of the diet of elderly Italians. II. Micronutrients. Int J Epidemiol 22:869–877
Cummings SR, Black G, McHenry K, Baron RB (1987) Evaluation of two food frequency methods of measuring dietary calcium intake. Am J Epidemiol 126:796–802
Kanis JA, Oden A, Johnell O, Jonsson B, De Laet C, Dawson A (2002) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12:417–424
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560
Michaelsson K, Melhus H, Bellocco R, Wolk A (2003) Dietary calcium and vitamin D intake in relation to osteoporotic fracture risk. Bone 32:694–703
Cumming RG, Nevitt MC (1997) Calcium for the prevention of osteoporotic fractures in postmenopausal women. J Bone Miner Res 12:1321–1329
Kanis JA, Johansson H, Oden A, Johnell O, De Laet C, Melton LJ, Tenenhouse A, Reeve J, Silman AJ, Pols HAP, Eisman JA, McClsokey EV, Mellstrom D (2004) A meta-analysis of prior corticosteroid use and fracture risk. J Bone Miner Res (in press)
Kanis JA, Delmas P, Reeve J, Garnero P, Tenenhouse A, Melton LJ, Oden A, McCloskey EV, Pols H, De Laet C (2003) A meta-analysis of previous fracture and fracture risk. Bone 32:S84
De Laet CEDH, Johansson H, Johnell O, Kanis JA, McCloskey EV, Mellstrom D, Melton LJ, Oden A, Delmas P, Garnero P, Oglesby A, Eisman J, Pols H, Reeve J, Silman A, Tenenhouse A (2003) A meta-analysis of body mass index as a predictor of fracture risk. J Bone Miner Res 18:S21
Kanis JA, Johnell O, Gullberg B, Allander E, Elffors L, Ranstam J, Dequeker J, Dilsen G, Gennari C, Lopez Vaz A, Lyritis G, Mazzuoli G, Miravet L, Passeri M, Perez-Cano R, Rapado A, Ribot C (1999) Risk factors for hip fracture in men from Southern Europe: the MEDOS Study. Osteoporos Int 9:45–54
Szulc P, Meunier JP (2003) Synergistic effect of vitamin D and calcium in preventing femoral fractures in older patients. Joint Bone Spine 70:157–160
Acknowledgement
We are grateful to the International Osteoporosis Foundation, the International Society for Clinical Densitometry, the National Osteoporosis Foundation, and the European Community (EU FP 3/5). We acknowledge the Alliance for Better Bone Health, Lunar, Hologic, IGEA, Lilly, Novartis, Pfizer, Roche and Wyeth for their unrestricted support of this work.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Kanis, J.A., Johansson, H., Oden, A. et al. A meta-analysis of milk intake and fracture risk: low utility for case finding. Osteoporos Int 16, 799–804 (2005). https://doi.org/10.1007/s00198-004-1755-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-004-1755-6