More than once last year, researchers described leaps in medical science that were so breathtaking, and held so much potential for patients, that they immediately joined the list of fields to watch in the year ahead. In most cases, the work was, and is, at an early stage and its future success far from certain. Such is the nature of science. Most of today's breakthroughs will be tomorrow's failures. But some may go down in history for transforming how medicine is done.
Often, medical science surges ahead when different areas converge. That's the case with genome editing, which gives scientists the extraordinary ability to rewrite genes in living organisms. At the heart of the process are enzymes that can sever DNA at chosen locations. But to be useful, it required advances in computational genetics, and exquisite techniques to manipulate biological cells.
Then there is the microbiome, the name given to the community of microbes that lives in and on our bodies. The trillions of bacteria that live in our guts, for example, influence our development, our metabolism, and our risk of scores of diseases. The prospect of treating, or preventing disease, through manipulating the microbiome, encouraging some bugs here, and fewer there, is a radical departure for medicine that now looks entirely realistic.
Cost is one of the greatest barriers to medical progress, so the falling price of genetic sequencing was bound to have an impact. Perhaps its most exciting application is the creation of gene profiles for tumours, which can be used to tailor therapies for individual patients. There is a long way to go, but solid progress has already been made.
These are only three of the most tantalising areas poised to make a major impact on medicine. Over the next year and more they may prove their worth, be superseded by better approaches, or fail spectacularly. Whatever the outcome, they are ones to watch.
Rewriting genes
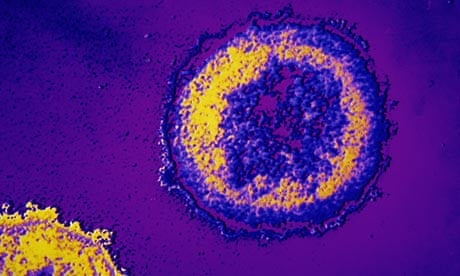
In 2009, doctors in Germany treated a man for leukaemia and in doing so cured him of HIV. Timothy Ray Brown was given a bone marrow transplant, a common enough option for leukaemia, but his donor was chosen specifically for a rare mutation in their cells. The genetic quirk, carried by a few per cent of the population, made the donor's white blood cells impervious to HIV. Once transplanted, the cells repopulated Brown's immune system, and made him resistant to the virus. He is the only person effectively to be cured of HIV.
The same approach cannot be used for the millions of others with HIV. There are too few appropriate donors, and the transplant operation alone carries a risk of death. But there might be another way, which draws on a technique called genome editing. The process is simple to explain, though complex to perform. First, extract immune cells from the patient. Then use enzymes to rewrite the DNA in those cells so they carry HIV-resistant genes. Finally, infuse the cells back into the patient. With luck, the modified immune cells thrive in the body, while the others die off.
The first clinical trial to do this in HIV patients ends this month. These are early days yet, and the trial will only assess safety, but the impact could be enormous. "This is one of the most exciting things I have seen," says Chris Mason, professor of regenerative medicine at University College London. "We don't know if it's going to work, but the potential is amazing."
The idea marks the convergence of two cutting-edge fields in medicine, namely gene and cell therapy. One advantage over traditional gene therapy is that the immune cells are modified in a petri dish, so they can be checked to ensure they are safe to return to the patient.
Genome editing may not work straight off the bat. But if the first trials go well – and more are already planned – then scientists will soon want to use it to tackle other diseases, such as haemophilia. "This is such a neat technique," says Mason. "Even if this is only applicable to HIV, just think of the numbers who could benefit."
Manipulating stomach bugs
You might think bacteria are our mortal enemies, but one of the hottest fields to emerge in medicine has firmly overturned that view. The microbes in and on our bodies can be our allies. They are intimately woven into our physiology and play a crucial role in our metabolism, development, and our susceptibility and response to diseases.
Last year, the Human Microbiome Project mapped the full community of microbes – the microbiome – that lurk in various parts of the healthy human body. Scientists are now finding that shifts in these bacterial groups raise or lower our risk of a staggeringly broad range of diseases. The reason is simple: the bugs release substances that are active in our bodies.
We carry more bacterial cells than human ones. A person's gut alone contains 100 trillion bacteria, or 10 times the number of human cells in the body. They hold several million genes, compared with the mere 20,000 or so needed to build and maintain a human being. Many scientists refer to the 1kg ecosystem of bugs as a "virtual organ" whose importance in medicine has long been overlooked.
In the year ahead, scientists expect to make headway in understanding the role of the microbiome in metabolic diseases, such as obesity and type II diabetes, and inflammatory problems, including colitis, Crohn's disease and irritable bowel disorder. Their findings could pave the way for radical new treatments that use drugs, or even specially tailored foods, to manipulate the microbiome, to prevent or cure diseases.
Cancer profiles
The cost of reading DNA has fallen to the point that doctors can take a biopsy from a tumour and see all of the mutations that triggered and drive the disease in an individual patient. Less than a decade ago, this was the stuff of science fiction.
The genetic histories of tumours that scientists can now piece together are crucial for grasping the basic biology of cancer, but also for efforts to improve cancer therapy. These profiles can tell doctors which drugs will work for a patient, and which are only likely to cause horrible side-effects.
To this end, the International Cancer Genome Consortium (ICGC) has begun sequencing the genetic code of 50 cancers in multiple patients, from brain and bladder, to lung and liver. For each disease, scientists want to define a genetic signature – the series of genes that mutate to cause the disease. For skin cancer, for example, there is a signature from exposure to ultraviolet light. In lung cancer, a common signature is produced by the chemicals in cigarette smoke.
Last year, the first results from the consortium were released to scientists worldwide. Far more will follow in the year ahead. "For each tissue type you can see the most commonly mutated genes," says Ultan McDermott at the Wellcome Trust Sanger Institute in Cambridge. "This gives us an unprecedented glimpse at what drives cancer, and tell us which pathways we should be targeting with drugs."
A separate project at the Sanger Institute, run by McDermott and others, is complementary to the ICGC's work. There, scientists are taking cells from cancer patients, growing them in the lab and exposing them to scores of old and new cancer drugs. The aim is to find drugs that are effective, even in only small groups of patients whose cancers are driven by specific mutations. In the years ahead, patients will increasingly be stratified – or broken down into smaller groups, according to genetic information – and treated with more bespoke drugs.
"There are probably many existing drugs that work but have not been tested in the right patients," says McDermott. "It may well be that we have a lot of the drugs we need, but simply don't know which patients to give them to."







Comments (…)
Sign in or create your Guardian account to join the discussion